PCF hosts an Annual Scientific Retreat to share the latest research findings, inspire collaboration, promote mentorship, and honor the newest awardees. Sessions at the 31st Retreat addressed basic biology and genetics research, clinical trials, new drug targets to overcome treatment resistance, the future of AI in prostate cancer, the impact of health habits on outcomes and survivorship, and more.
Decades ago, PCF was an early supporter of research on the relationship between diet and prostate cancer outcomes. This field has advanced considerably, although much more remains to be discovered.
Dr. Stacey Kenfield of UCSF and Dr. David Nanus of Weill Cornell Medicine presented the latest updates.
- Health habits: Current data suggests that patients can take actions to improve their survivorship with prostate cancer and overall health through aerobic exercise, strength training, and following dietary patterns emphasizing plant-based foods and the Mediterranean diet
- Clinical trials: For overweight & obese patients on hormone therapy, a whole-food, plant-based diet shows promise in overcoming metabolic side effects of the treatment
Impact of Exercise and Diet on Prostate Cancer Outcomes
Stacey Kenfield, ScD
University of California, San Francisco
Dr. Kenfield discussed the relationship between aerobic physical activity and clinical outcomes in patients with prostate cancer.
The first study in men diagnosed with prostate cancer demonstrated that moderate levels of total physical activity (about 30 minutes of walking most days per week) were associated with reduced overall mortality, while higher levels of vigorous physical activity (about 1 hour or more per day of jogging) were associated with reduced prostate cancer-specific mortality. Additional studies include cohorts from the US, Sweden, and Canada, and include people across the disease spectrum of stage and grade. Benefits from these studies were also seen at more modest levels of activity. For example, walking and biking at levels of 20 min/day or more were associated with a lower risk of overall mortality and prostate cancer-specific mortality.
These study findings, taken together, consistently show a beneficial association of exercise after diagnosis with prostate cancer outcomes and have led to an update to the Physical Activity Guidelines for Americans in 2018, which now states that prostate cancer survivors have a lower risk of dying of prostate cancer with regular physical activity.
The guidelines recommend at least 150 minutes a week of moderate-intensity aerobic physical activity or at least 75 minutes of vigorous-intensity aerobic physical activity, or an equivalent combination. These guidelines also recommend muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on 2 or more days a week, and balance training as separate component. Studies have also found that fitness and muscle mass are associated with improved outcomes in men with prostate cancer.
INTERVAL-GAP4 is an ongoing randomized study coordinated at USCF and Edith Cowan University which aims to determine if supervised exercise (vs. self-directed exercise) improves overall survival in patients with metastatic prostate cancer. Results from this study will be available in 1-2 years.
Dietary patterns and scores have also been associated with prostate cancer outcomes.
The Western dietary pattern has been associated with increased prostate cancer-specific mortality and overall mortality, while the prudent and Mediterranean dietary patterns were associated with lower overall mortality. The prudent dietary pattern is characterized by higher intake of legumes, vegetables, fruits, whole grains, garlic, soy products, fish, and oil-and-vinegar dressing. The Mediterranean dietary pattern is characterized by high intakes of vegetables, fruits and nuts, legumes, cereals, fish and seafood, high ratio of polyunsaturated to saturated fat, 10-50 g/day of alcohol, and low intake of red and processed meats, and dairy products.
A plant-based diet (eating more plant-based foods versus animal foods) was associated with lower risk of prostate cancer progression. The Healthy Plant-Based Diet index, which gives negative points to foods including fruit juices, sugar-sweetened beverages, refined grains, potatoes, and sweets and desserts, has been associated with lower risk of prostate cancer progression among patients with Gleason Grade 7 and higher prostate cancer.
Prostate-8-II is an ongoing study which aims to determine the effect of a digital health behavioral intervention on clinical, patient-reported, and biological outcomes in patients with prostate cancer who had surgery.
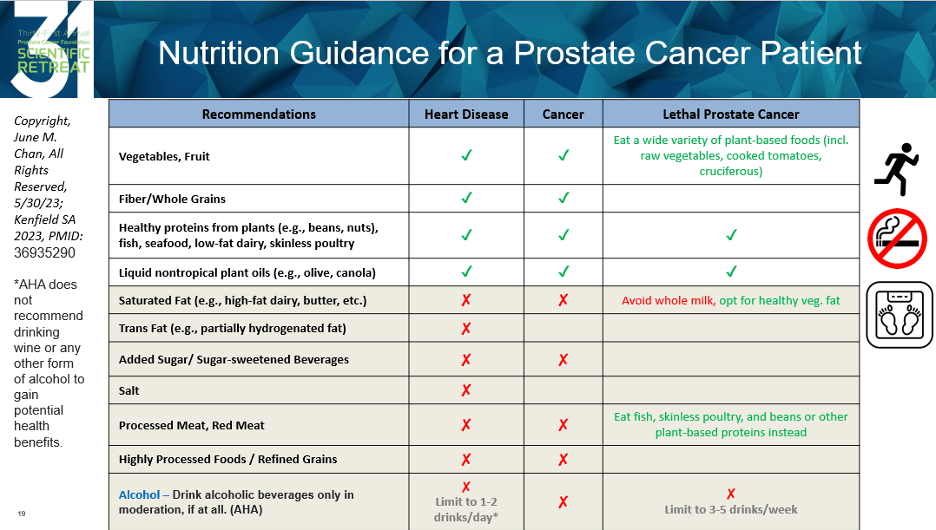
Overall, recommendations of modifiable health habits to improve prostate cancer outcomes and quality of life include regular physical activity, smoking cessation, and maintaining a healthy body weight. While evidence is less consistent on the impact of diet and specific foods, the data suggest avoiding Western pattern foods and eating more plant-based and Mediterranean diets for overall health, and following nutrition guidelines for heart disease and cancer prevention with some modifications specific for patients with prostate cancer (see Figure below).
Updates on a Clinical Trial of a Whole-Food Plant-Based Diet in Men Receiving ADT
David Nanus, MD
Weill Cornell Medicine
We’ve written extensively about a clinical trial exploring the potential benefits of a whole-food plant-based diet to improve weight as well as measures of metabolism and inflammation in overweight/obese patients with prostate cancer receiving androgen deprivation therapy (ADT, or hormone therapy). ADT is a mainstay of treatment for high-risk and metastatic prostate cancer, but often causes weight gain, loss of muscle mass, increased cholesterol, and other impacts on metabolism and the gut microbiome. Overweight and obese patients on ADT need practical, sustainable interventions to promote weight loss, lower inflammation, and improve cardiovascular health and metabolism. You can read more about this trial here.
Dr. Nanus presented an update: 46 patients have been enrolled thus far. In preliminary results, patients on both trial arms were observed to lose weight, with patients on the plant-based diet arm experiencing significantly greater weight loss, and greater decreases in body mass index (BMI) and fat mass. Weight loss in most patients persisted at 6 months. Related studies, including analysis of the gut microbiome, are ongoing.
These data provide promising indications that a whole-food plant-based diet may improve health outcomes in patients with prostate cancer treated with ADT.









